A surgery that plants electrodes deep inside the brain is bringing new hope to people with Parkinson's disease here in Ottawa.
It's called "deep brain stimulation" and the effect for one patient that CTV Ottawa interviewed was astonishing.
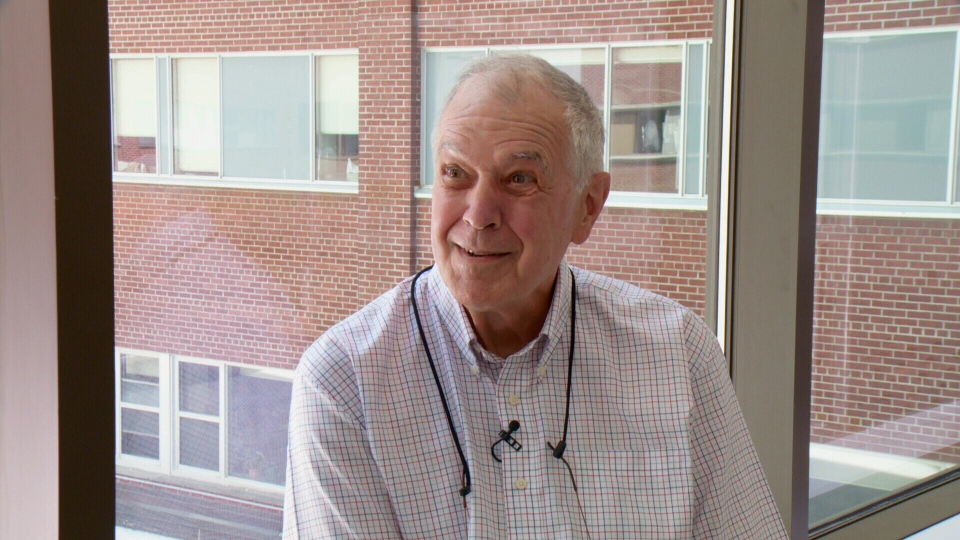
Dr. Jacques Theriault was diagnosed with Parkinson’s in May of 2006. His tremors were so profound that he quit his family medicine practice the day after he was diagnosed. With the disease progressing and his medication intake now up to 19 pills daily, Dr. Theriault was looking for other options. On the internet, he found something called Deep Brain Stimulation or DSB, and then discovered that the Ottawa Hospital had just started doing the procedure here. Dr. Theriault demonstrated for our camera what happens when he shuts off the stimulator that is activating the DSB electrodes. Within seconds, his tremor reappears.
‘I’m not doing this on purpose,’ says Dr. Theriault, unable to control the violent jerking of his right arm, ‘It’s worse on my right side as you can see.’
With a click of a button, similar to a TV remote control, the tremor stops just as dramatically as it began.
‘Isn’t it amazing?’ he says, with a big grin.
Parkinson's took away Dr. Theriault's ability to practice family medicine, but this surgical procedure here in Ottawa has given him back his quality of life, at least for now.
‘I’m off my medications altogether,’ he says, ‘19 pills a day I don't have to take, with all their side effects.’
The Ottawa Hospital just started doing "Deep Brain Stimulation" or DBS about a year ago.
The patient in the operating room at the Ottawa Hospital is patient number 19. He is awake during the procedure.
‘The goal of DBS,’ says Dr. Adam Sachs, the neurosurgeon who is performing the surgery here, ‘is to improve motor symptoms and reduce fluctuations with those medications and usually reduce the dose of medications they are on.’
DBS was developed in France in the 80's. It involves implanting electrodes deep in the brain through small holes in the skull that are connected to a "stimulator" similar to a pacemaker. The stimulator sends electrical signals down those electrodes in the brain to a very precise spot that is affected by Parkinson's disease, usually the subthalamic nucleus.
‘The patient has to be awake because they will be reporting the symptoms they are having,’ explains Dr. Sachs.
When the surgeon hits the right spot with the micro-electrode, the neurons are fired and the operating room team can actually hear that reaction in the brain. Once they find that "sweet spot" on both sides of the brain, a "deep brain stimulation” electrode permanently goes in, connected by a thin wire that runs under the skin, down the neck and into a battery-powered stimulator under the skin in the chest.
Not everyone with Parkinson's disease is a candidate for this procedure. They are carefully tested and selected. Dr. Tiago Mestre is the Ottawa Hospital neurologist who does that testing.
‘Patients with Parkinson’s must have been treated,’ he explains, ‘and knowing that they respond to medications is usually a good prognosis.’
Dr. Mestre says patients are usually considered for this procedure when they develop motor complications that involve uncontrollable involuntary movements or when their medications are no longer lasting as long. DBS is also used for patients with dystonia or essential tremor.
‘We are able to give them back a fair good quality of life and that's what they appreciate,’ he says, but cautions that this is not a cure for the disease but rather a remission, perhaps for 3 to 5 years.
Clearly, the results for some, including Dr. Jacques Theriault, have been dramatic and life-changing. Dr. Theriault says he was going to be in a wheelchair within six months and could no longer drive. That prognosis has changed.
‘It’s a technological miracle,’ he says.