After five deaths in one week by suspected drug overdoses, CTV Ottawa brings you an in-depth look into Ottawa’s growing opioid crisis. Over three days we’ll look at the people struggling with drug addiction, the daily fight for survival and why some say a safe drug supply may be the only way to save lives. This is Part 3.
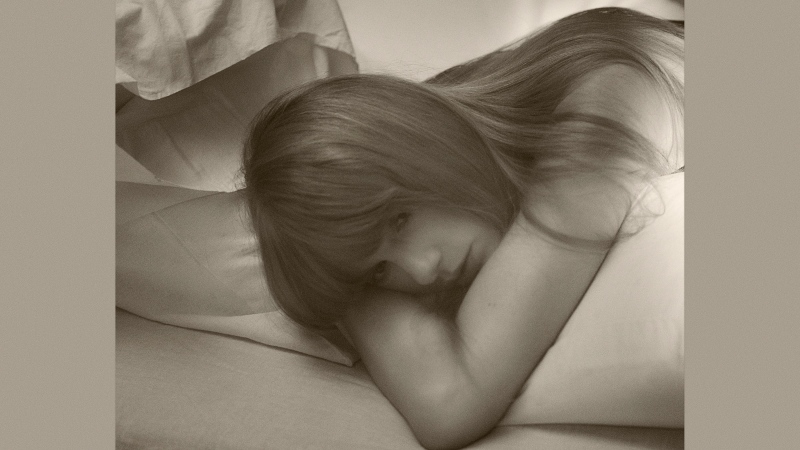
Jenn’s Story:
When Jenn Sabourin, 45, sits back and reflects on the years gone by what she sees is difficult to absorb.
“It’s a waste, really. I wasted my life.”
Jenn has been using drugs since she was 13 years old: more than 30 years of life on the edge.
“I was doing whatever I could to get money to be high every day.”
Jenn says she was using recklessly and alone.
“I had OD’d three times in a week and a half. I had no place to live, my family had just had it, and I had nothing you know.”
r’s story: (CTV has agreed to protect his identity)
When r was 18 years old in his hometown of London, Ont., ‘dabbling’ in drugs like crystal meth, he could never have predicted this life.
“Slowly you realize this thing you think is fun, this thing you think is helping you get through your life is actually destroying everything you’re building and trying to work for.”
That’s when the spiral began. The “dabbling” turned to addiction. He moved to Ottawa and his drug of choice wasn’t just crystal meth anymore, instead heroin and toxic street opioids.
“I quit a number of substances without any trouble but there’s no way I could stop using opioid.”
He blames the crisis and overdoses on street drug producers who, r says, are purposely lacing all kinds of street drugs, not just opioids, with highly addictive fentanyl and carfentanil.
“For people to be buying crack and having fentanyl show up in it is completely ridiculous,” r says. “They’re going to become addicted to something they don’t even know they’re smoking. That’s horrible. Who takes advantage of somebody like that? Whoever they are, they need to stop because they’re killing people.”
A year ago, after overdosing, r thought at any moment the drugs would kill him.
“It was only a matter of time before I was somewhere alone without somebody to help me.”
MOP:
About a year ago, Jenn and r were both desperate for help.
“I OD’d and ended up in the hospital,” Jenn says. “One of the workers met me at the hospital and brought me home and I started the program that day.”
It’s called the Managed Opioid Program (MOP) run by Ottawa Inner City Health. The first of its kind in the world, MOP, is a residential opioid replacement therapy. Ten patients, including Jenn and r, agreed to give up risky opioid street drugs in exchange for a place to live, mental and physical support, and daily doses of doctor prescribed hydromorphone.
“It’s been shown that the injection drug users don’t know, can’t really determine, the difference between hydromorphone and heroine,” says Dr. Jeffrey Turnbull, the former Chief of Staff at the Ottawa Hospital who quit the top job to care for the city’s homeless.
Dr. Turnbull and Ottawa Inner City Health Executive Director Wendy Muckle run the program. MOP costs $8,628 per person per year. Dr. Turnbull says that is a relatively small price to pay considering the alternative.
“We’re paying so much money to incarcerate people with mental health issues and addictions. Shelters, healthcare, hospitals and emergency services are all hugely expensive.”
They say a safe supply of drugs may be the only way out of this crisis. The current street drugs are so addictive, just asking users to quit or enter 30-day treatment programs they say not an option.
“No supply is better, but the practicality of moment is at least it has to be safe,” says Dr. Turnbull.
“We’ve said okay: we will give you safe, prescribed opioids, we’ll do it in a controlled fashion and once you’re stable in a housed environment we’ll start treating your mental health problems and we’ll start to treat your physical health problems and we’ll talk about education, schooling, we’ll talk about employment, all of those things as a road to recovery.”
In the year the program has be going they say there has been success. Patients like Jenn and r, even though they’re still injecting every day, are starting to see the potential of a life that may not include drugs.
“Once you can move someone from the crisis of their day, their personalities emerge and they stop being that person that you and I want to walk around on the street and start becoming somebody’s son, brother and father,” says Dr. Turnbull.
“I’m here, I’m not committing crimes everyday just to get my fix,” says r, “I’m an artist, and I’m a musician and a lot of other things. You forget about these things, you forget to read books and paint pictures and play music. You get lost in yourself and it’s not good to get lost in when there’s not much going on inside you.”
“My whole life I’ve been nothing but a drug addict and a junkie. Now I’m just a patient with medication. I was looked at as a human being again.”
Jenn admits the struggle is still very real every single day.
“I’m an addict, right? So that takes over sometimes but I don’t use like I used to,” she says. “I’m beginning to have a relationship with my children, before I didn’t; it’s still a slow process.”
There is a long wait list for others to join MOP; the concern is they could die before making it into the program. While Muckle is pushing government for funding to expand MOP, she says there is a more efficient, cost effective way to help all injection drug users immediately. She says offering a safe supply of drugs to users at their current supervised injection site on Murray Street would save lives.
“If people were coming through the door here at the Supervised Injection Site and can all be offered legally prescribed medications you know we already exist, the staffing is already here, it would be relatively cheap to be able to do that.”