The Ottawa Hospital and the city of Ottawa are teaming up to launch a new program aimed at helping first responders deal with mental health issues.
It's a first of its kind in Canada and couldn't come at a time of greater need.
Whether it’s a collision with multiple fatalities or a violent murder, it is the kind of carnage those first on the scene never forget. Sure, it's part of the job for first responders but a part that takes a heavy toll.
Sergeant Brent MacIntyre knows that all too well. He was a front-line officer for many years and now is with the Ottawa Police Peer Support program, working with officers dealing with traumatic experiences.
“That's something that never leaves any of these officers and something you have to come to terms with it and some never do,” says MacIntyre
Staff-Sergeant Kal Ghadban's suicide 4 years ago at the Ottawa Police Headquarters hit his police family hard. His colleagues couldn't understand how they hadn't seen this coming, how they might have missed signs of depression in their friend.
Mental health issues are skyrocketing among first responders. Research from the Canadian Institute for Public Safety Research and Treatment shows that 45% of first responders in Canada have symptoms consistent with at least one mental health disorder. That’s about four times higher than in the general population. A related study found that nearly one-third of first responders in Canada have had thoughts of suicide, double the rate in the general population.
“If they had an opportunity to visit a proper clinician,” says MacIntyre, “somebody who got it, who worked with first responders, we could swim upstream, get them before they saw no other option than to take their life.”
And that's the aim behind a new project in Ottawa that looks at setting up a mental health clinic specifically designed for first responders. The city of Ottawa is championing the new study, led by researchers at The Ottawa Hospital and the University of Ottawa. It’s a two-phase project, first to see what first responders want, then to set up a research-based mental health clinic to do a pilot randomized controlled trial to test its effectiveness over a one year period.
Dr. Simon Hatcher is the principal investigator on the project and a Psychiatrist at The Ottawa Hospital.
“What I hope,” he says, “is that we will have a clinic which is acceptable to first responders, that provides timely care and care which is effective.”
The federal government, through the Canadian Safety and Security Program, is providing $462,000. The project could become a model for Canada. The plan is to launch the clinic in the spring. There's funding initially for about 40 people. What the demand will be isn't clear but there's definitely a growing need.
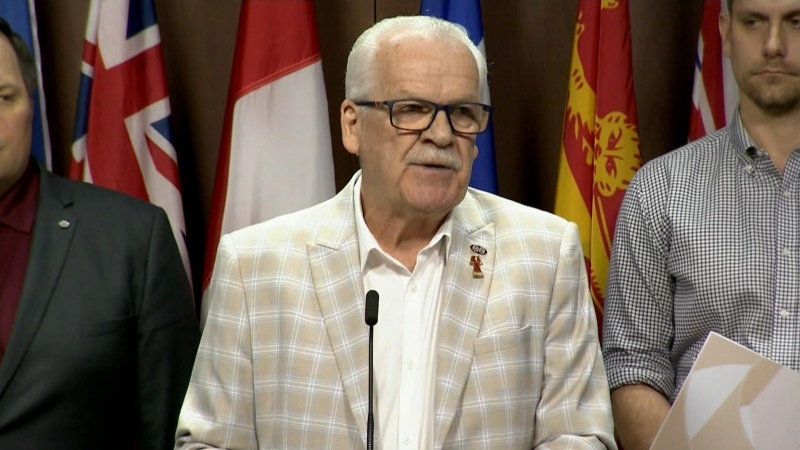
Ottawa's Head of Emergency and Protective Services says the challenge will be encouraging first responders to reach out for help.
Providing first class care is now a priority, says Anthony Di Monte.
“These people put their lives on the line every day for our community and this is the minimum they deserve,” he says.